Unlocking Behaviors: Gastrointestinal Distress
Co-written by Risley “Ley” Linder, MA, MED, BCBA & Craig Escudé, MD, FAAFP, FAADM
This article is part of a co-authored series on behavioral presentations in which a physician and a behavior analyst provide insight into real-life case studies to share their expertise on how behavioral issues can be addressed in an interdisciplinary fashion.
Rick is a 43-year-old man with a moderate intellectual disability. He is very active and is described as a “high-energy” person. He was transferred to a new group home after his last one closed due to the inability to find enough staff to meet the needs of the people they supported. It was immediately noted by the new support team that Rick frequently searched for things to eat, and most of it was not food. He would look for objects on the ground, find whatever he could, and eat them. A repairman was working on the heater, and Rick managed to grab a small screw and swallow it before anyone could stop him. There was a tear in the vinyl flooring in his room, and staff noted one morning that the tear was a bit larger. Later, they saw him picking the flooring, breaking small pieces off, and eating them.
His staffing needs increased to monitor him more closely and prevent him from ingesting harmful objects. His level of aggression began to increase as staff would attempt to keep him from eating non-food items.

Photo Credit: 2023 Rick Guidotti, Positive Exposure. All Rights Reserved.
Medical Discussion
Eating things of non-nutritional value or non-food items is called pica. People may search for objects on the ground, pull stuff off the wall, or constantly search for some object to chew or swallow. It is more commonly seen in children, pregnant women, and people with conditions such as autism, intellectual disabilities, and schizophrenia. Many forms of pica involve one particular item that a person ingests.
Examples include:
- Chalk
- Clay
- Dirt
- Coffee grounds
- Ice
- Paper.

Sometimes pica is associated with underlying medical conditions. One of the more commonly seen conditions in the general population is iron deficiency which may be associated with an ice pica.
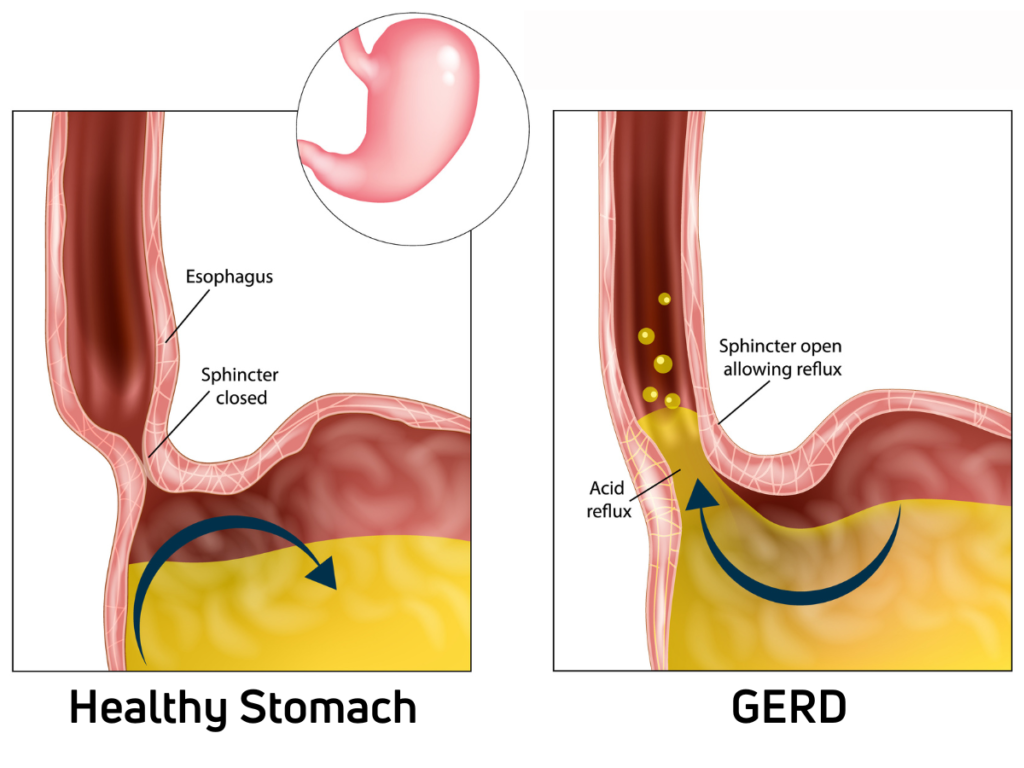
In people with intellectual and developmental disabilities, a condition that is noted to be commonly associated with pica behavior is gastroesophageal reflux disease (GERD). One suspected reason for this association is that a person learns that if they swallow more frequently, the acid that causes the pain is washed back into their stomach. They then begin looking for items to eat to stimulate salivation to wash down the acid.
Another commonly seen presentation of GERD is someone who likes to chew on a sock or other object. If you support someone who does this or has pica behavior, you might consider asking for an evaluation for GERD. They may be chewing to stimulate salivation to wash the acid down to relieve pain. Consideration should also be given to checking for Helicobacter Pylori infection, which has been implicated as a cause of GERD.
Behavioral Discussion
When examining pica behaviors, the first question is, “Are there immediate health and safety concerns?” As a few quick examples, is the person in immediate danger from consuming toxic chemicals, uncooked food, sharp items, or unknown items/substances? If so, medical assistance should be sought immediately.
Second, “What is the historical dynamic of this behavior?”
In the case of Rick, long-term pica behaviors can result from undiagnosed/untreated medical conditions in conjunction with learned behaviors that actually have logic in their engagement.
To continue with Dr. Escudé’s point, if a person consumes the brittle, chalk-like substance comprising drywall, they can learn that this eases the discomfort in their stomach, throat, and mouth (e.g., GERD symptoms). The presentation we, as behavior analysts hear is, “They are eating the walls!” In reality, they have found an “antacid” in their environment that is managing the discomfort they are experiencing.
Behaviorally, pica behaviors should be presumed to require a multidisciplinary approach until proven otherwise. The rare but eye-catching “Rapunzel Syndrome” illustrates how pica behaviors are complex and require insight from various professionals. The combination of trichotillomania (pulling out your hair) and trichophagia (chewing/consuming hair) requires a multi-faceted plan of care that requires behavioral management, psychiatric consultation for potential underlying diagnosis, routine primary care check-ups, and crisis management for potential medical needs – to name a few.
Chronic pica behaviors can be reduced, particularly if the underlying cause is related to a medical condition. However, the person may still exhibit the pica behavior “out of habit.” Using the example of a person consuming drywall, they have learned that this behavior effectively alleviates the discomfort they feel. At the beginning of treatment (e.g., taking medication), they may continue to engage in the behavior, as they have to learn that taking medication is a more effective means of reducing discomfort. The person should be monitored after the introduction of a medication to see if the behavior decreases, stops, or even increases, as the medication type, dosing, or other factors may not be the “right fit.” In other words, if the medication is ineffective in reducing the discomfort, the pica behavior will likely continue.
If the behavior abates after the introduction of any intervention (e.g., medical and/or behavior) but suddenly re-appears, there could be an acute stimulus that is exacerbating the existing diagnosis and should be evaluated by a medical professional. The pica behavior should also be considered as potentially indicating other medical concerns as the person may have generalized the pica behaviors using the logic, “Well, this helped me the last time my stomach hurt.”
Outcome
Thanks to an astute direct support professional and a responsive team that was aware of the association between pica and GERD, Rick was taken to see a gastroenterologist who performed an endoscopy. He noted numerous gastric and esophageal erosions consistent with GERD. Rick was started on a proton pump inhibitor, and over the next several weeks, his pica behavior slowly lessened. His suffering from GERD symptoms, his overall health risk, and the need for additional staffing were all reduced, resulting in improved quality of life for Rick, his supporters, and the support agency.
Author Bio:
Ley is a Board-Certified Behavior Analyst with an academic and professional background in gerontology and applied behavior analysis. Ley’s specialties include behavioral gerontology and the behavioral presentations of neurocognitive disorders, in addition to working with high-management behavioral needs for dually diagnosed persons with intellectual disabilities and mental illness. He is an officer on the Board of Directors for the National Task Group on Intellectual Disabilities and Dementia Practices, works closely with national organizations such as the National Down Syndrome Society, and is the owner/operator of Crescent Behavioral Health Services based in Columbia, SC.
Dr. Craig Escudé is a board-certified Fellow of the American Academy of Family Physicians and the American Academy of Developmental Medicine and President of IntellectAbility. He has over 20 years of clinical experience providing medical care for people with IDD and complex medical and mental health conditions. He is the author of “Clinical Pearls in IDD Healthcare” and developer of the “Curriculum in IDD Healthcare,” an eLearning course used to train clinicians on the fundamentals of healthcare for people with IDD. He is also the host of the “IDD Health Matters” podcast.




