Unlocking Behaviors: Dental Health
Unlocking Behaviors: Dental Health
Co-written by Risley “Ley” Linder, MA, MED, BCBA & Craig Escudé, MD, FAAFP, FAADM
Published by Helen Journal
This article is part of a co-authored series on behavioral presentations in which a physician and a behavior analyst provide insight into real-life case studies to share their expertise on how behavioral issues can be addressed in an interdisciplinary fashion.
When it came to tennis, 37-year-old Tim was a huge fan. He loved watching how fast the players hit the ball back and forth, especially his favorite player Roger Federer. He knew the general timing of the US Open and other major tennis events and would watch as many matches as possible.
Tim enjoyed snacking on almonds and other nuts while watching tennis. One year, during the US Open, he decided he didn’t want almonds and even knocked them off the table a couple of times. He began to get a bit agitated at various times of the day or night, and his support staff wasn’t sure what was going on. After a few weeks, Tim became quite a challenge, hitting out at others, wanting to stay in his room more, and even eating less.
Tim was taken to his primary care physician for an evaluation. He underwent a physical exam, and nothing unusual was found except for a 5-pound weight loss since his last visit six months prior. Because of his agitation, he was then seen by a psychiatrist. Staff were concerned that he was endangering himself and others during his episodes of agitation. He was started on psychotropic medication in an attempt to reduce his aggression. It seemed to work for a while, but then the agitation ramped up again. After several psychiatry visits and medication adjustments, the recommendation was made to move Tim to an in-patient psychiatric setting for evaluation.
A relatively new nurse who had recently attended a conference about behavioral changes in people due to underlying medical conditions attended Tim’s final team meeting before he was to be committed. She recalled hearing at the conference how dental issues can cause agitation. She recognized that Tim had not had a dental evaluation in the last three years because of COVID restrictions and his inability to wear a mask.
Medical Discussion
Primary care physicians are not dentists. (No surprise there). But in the situation described above, primary care clinicians are often asked to evaluate a person with a change in behavior to rule out underlying medical causes. Most people, if they have tooth pain, automatically know to see a dentist and don’t show up at the family physician’s office for an evaluation. But for many people with a limited ability to use words to communicate, agitation is often the first indicator of discomfort, and the initial assessment is usually by a primary care clinician or a psychiatrist. Primary care clinicians aren’t necessarily used to thinking about dental causes of pain because most people will go to the dentist first.
Anything that causes pain in a person’s mouth can make them agitated around mealtimes (due to the anticipation of pain with chewing). They can also spit out food, prefer soft foods over crunchy foods, refuse to go to the dinner table, refuse oral care, and can even be aggressive.
Behavioral Discussion
Tim’s decreased desire to snack on nuts and watch the greatest tennis player of all time is an entirely preventable situation. Dr. Escudé listed a few behaviors that can happen when a person has pain and/or discomfort in their mouth. It’s important to recognize these types of behaviors, but Tim’s situation allows us to discuss another area of behavior: acute vs. chronic behaviors.
Acute vs. Chronic Behaviors
Tim’s preference for snacking on nuts and watching tennis is something that had occurred for many years, and there was an acute change in behavior.
Tim’s acute change in behavior was characterized by changes in:
- Preferences
- Routines
- Medical issues, such as unintended weight loss.
Sudden changes in behavior and/or new behaviors are more likely to happen because of changes in a person’s environment (e.g., new job) or medical issues (e.g., toothache), as opposed to more chronic issues (e.g., psychiatric symptoms).
For Tim, having never been prescribed psychotropic medications, the acute onset of psychiatric symptoms in middle age is not a likely cause for the change in food and activity preferences.
Observing and Assessing
When observing and assessing acute onset behaviors, thinking about three key areas is important.
- First, has anything changed in their environment? Can we clearly identify a change that would account for the rapid change in preferences?
- Second, what is the timeline of changes? When did the behavior change(s) start? Sometimes using events instead of time to track changes can be helpful. For example, “Tim was eating nuts while watching Wimbledon in July, but he wasn’t during the US Open in August. What could have happened in the last month?”
- Lastly, it’s important to note if the behaviors happen across time, setting, and people. If they only happen at one particular time, in a specific setting, or with certain people, they are more likely to be environmental, as opposed to medical-based behaviors that are more likely to happen across time, settings, and people.
Outcome
The nurse recalled what she learned at the conference and recommended that Tim have a dental evaluation before being admitted to the psychiatric hospital. Tim was found to have several abscessed teeth. After they were all treated, his pain resolved. They tapered off his psychotropic medication, and he made up for all the tennis he missed— and the eating. Tim avoided a psychiatric admission and likely additional psychotropic medicines because of the nurses’ insistence on a dental evaluation.
The Authors
Risley “Ley” Linder
Ley is a Board-Certified Behavior Analyst with an academic and professional background in gerontology and applied behavior analysis. Ley’s specialties include behavioral gerontology and the behavioral presentations of neurocognitive disorders, in addition to working with high-management behavioral needs for dually diagnosed persons with intellectual disabilities and mental illness. He is an officer on the Board of Directors for the National Task Group on Intellectual Disabilities and Dementia Practices, works closely with national organizations such as the National Down Syndrome Society, and is the owner/operator of Crescent Behavioral Health Services based in Columbia, SC.
Dr. Craig Escudé
Dr. Craig Escudé is a board-certified Fellow of the American Academy of Family Physicians, the American Academy of Developmental Medicine, and President of IntellectAbility. He has more than 20 years of clinical experience providing medical care for people with IDD and complex medical and mental health conditions. He is the author of “Clinical Pearls in IDD Healthcare” and developer of the Curriculum in IDD Healthcare,” an eLearning course used to train clinicians on the fundamentals of healthcare for people with IDD.









 Health-related Resources for People with IDD and Their Supporters
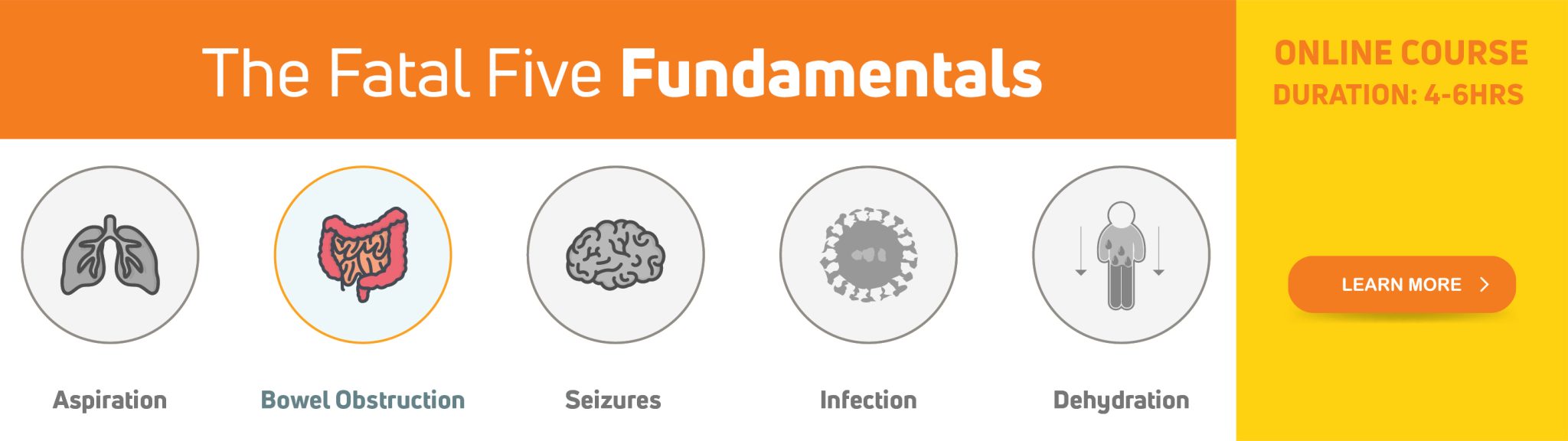
Health-related Resources for People with IDD and Their Supporters With significant health disparities noted in people with IDD, it is important that people with intellectual and developmental disabilities (IDD), their supporters, and healthcare providers educate themselves on the different health risks that are more commonly seen in people with IDD and about what can be done to prevent serious complications. Supporters and healthcare providers are often challenged in finding helpful information related to healthcare for people with IDD. As a physician who started practicing in this field in the 1990s, finding clinically relevant information about healthcare for people with IDD was challenging. Fortunately, over the past several years, more resources have been developed that relate specifically to healthcare issues and improving health equity for people with IDD. In this article, you’ll find a listing of websites, tools, and training available to provide information and guidance to you, whether a family member, paid supporter, healthcare provider, or person with IDD.
With significant health disparities noted in people with IDD, it is important that people with intellectual and developmental disabilities (IDD), their supporters, and healthcare providers educate themselves on the different health risks that are more commonly seen in people with IDD and about what can be done to prevent serious complications. Supporters and healthcare providers are often challenged in finding helpful information related to healthcare for people with IDD. As a physician who started practicing in this field in the 1990s, finding clinically relevant information about healthcare for people with IDD was challenging. Fortunately, over the past several years, more resources have been developed that relate specifically to healthcare issues and improving health equity for people with IDD. In this article, you’ll find a listing of websites, tools, and training available to provide information and guidance to you, whether a family member, paid supporter, healthcare provider, or person with IDD.

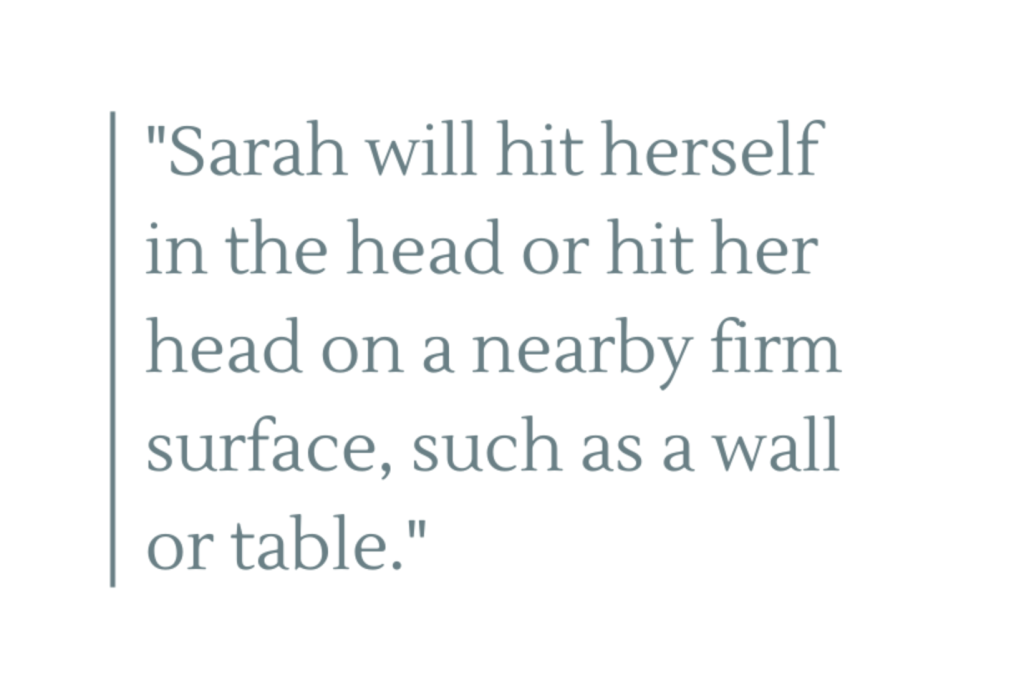
 Mitchell was taken to the ER because his supporter noted that he was becoming noticeably agitated, was refusing to eat and had begun biting his arm intermittently. His supporter, who knew him well, recalled how he had done this a few times in the past, and most of the time, he was eventually found to have some underlying condition that caused him discomfort. Unfortunately, on some of those previous occasions, it took several clinician visits to get to the right diagnosis.
Mitchell was taken to the ER because his supporter noted that he was becoming noticeably agitated, was refusing to eat and had begun biting his arm intermittently. His supporter, who knew him well, recalled how he had done this a few times in the past, and most of the time, he was eventually found to have some underlying condition that caused him discomfort. Unfortunately, on some of those previous occasions, it took several clinician visits to get to the right diagnosis.


