Unlocking Behaviors: Constipation
IT’S HELPFUL TO KNOW WHAT SOME OF THE MORE COMMON CAUSES OF A CHANGE IN THE LEVEL OF ALERTNESS OR ACTIVITY (“NOT ACTING RIGHT”) CAN BE. AND FOR PEOPLE WITH IDD, ONE OF THE MOST COMMONLY SEEN CAUSES IS CONSTIPATION. I 8 MIN
Co-written by Risley “Ley” Linder, MA, MED, BCBA & Craig Escudé, MD, FAAFP, FAADM
Published by Helen Journal
This article is part of a co-authored series on behavioral presentations in which a physician and a behavior analyst provide insight into real-life case studies to share their expertise on how behavioral issues can be addressed in an interdisciplinary fashion.

Ron is a 41-year-old man with a severe intellectual disability. He recently moved into a group home after having lived with his parents for most of his life, but because of health issues in both of his aging parents, they can no longer provide the level of support he needs. Ron uses few words but can mostly make his needs known through gesturing and limited sign language. He eats and goes to the bathroom on his own. He loves watching baseball on TV and goes to games at the local minor league stadium when he can. He gets pretty excited when the game comes on and sometimes won’t eat because of his excitement. Overall, he is adjusting well to his new living arrangement, but he seems to be missing his parents, especially when the games come on TV, as he used to watch them with his dad.
Over a period of 3 days, Ron seemed to have become less active. He began sitting more of the day, sometimes pulling his knees up to his chest when in the chair. He started eating less, as well. The “big game” was set to air in a few hours, but Ron wasn’t very interested in it. This was unusual for Ron, and the staff brought it to the nurse’s attention.
Medical Discussion
One of the most common chief complaints provided by a supporter of a person with IDD during an office visit or an emergency department visit is “He’s just not acting right.” For many clinicians, this leaves the door wide open for the reason being something simple and easily treatable to something as much more severe and potentially life-threatening. It’s helpful to know what some of the more common causes of a change in the level of alertness or activity (“not acting right”) can be. And for people with IDD, one of the most commonly seen causes is constipation.
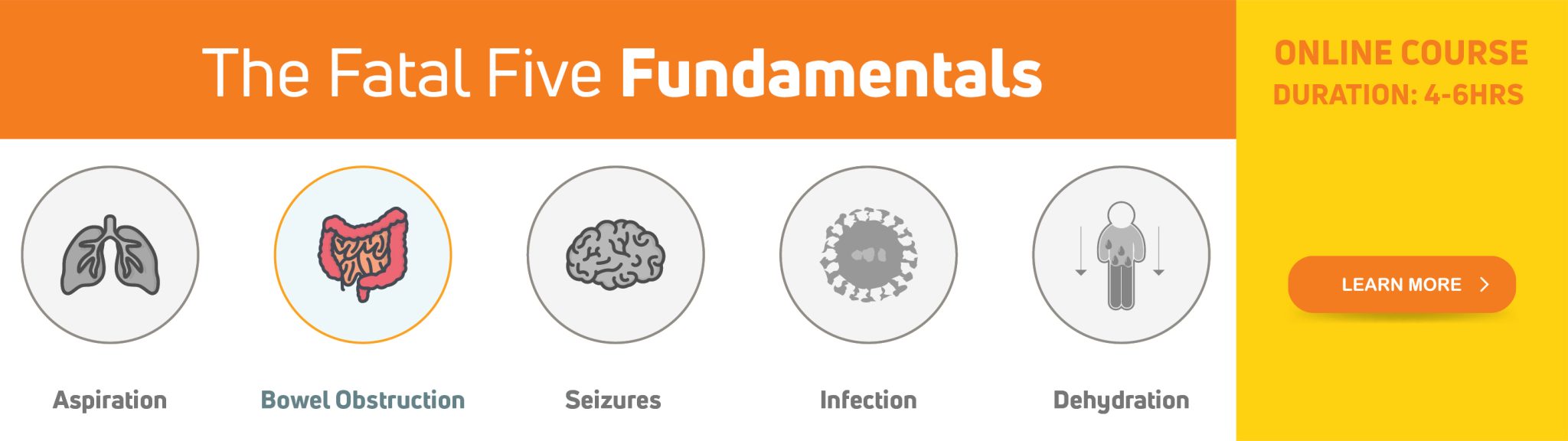
Constipation is one of what we call the “Fatal Five,” the top preventable causes of illness and death in people with IDD.
Constipation can cause a wide range of symptoms, including:
- Lethargy
- Lack of interest in usual activities
- Not wanting to eat
- Sitting or lying with the knees brought up to the chest or curled in a ball
- Abdominal guarding
- Restlessness
- Aggression without any apparent reason.
I’ve been frequently known to say, “Think about constipation first,” as it can be a common cause of an acute change in behavior.
In addition to changes in behavior, I’ve noted other changes, including:
- Low-grade fever
- Vomiting
- For a person with a seizure disorder, an increase in their seizure frequency.
On multiple occasions, I’ve had patients experiencing an acute increase in seizure activity who were found to be constipated. Once the impaction was resolved, their seizure pattern when back to baseline. Because of this, our standard practice was to check for an impaction when they presented with a seizure flurry.
Constipation is one of what we call the “Fatal Five,” the top preventable causes of illness and death in people with IDD.

Why is constipation such an issue for people with IDD?
There are several reasons, including that many medications people are more likely to take can cause anti-cholinergic effects, which can dry things up and slow things down. Slowing transit through the intestine allows for increased water absorption, which firms up the stool. Movement of large muscle groups helps stimulate bowel activity, and for some, this may be limited. Inadequate fiber and fluid intake can negatively impact bowel regularity. And some with pica behavior may ingest non-food items that can cause bowel blockage.
Behavioral Discussion
From a behavioral standpoint, when we work with individuals with limited or highly idiosyncratic communication skills who are exhibiting acute changes in behaviors, particularly ones that can be described as “odd,” “different,” or “not acting right,” we always want to know if the behavior has occurred before. For Ron, has he engaged in this type of change in positioning/posturing behavior in the past? If so, what was the outcome or resolution? Was there a clear cause and specific intervention that led to the cessation of the positioning behavior (and subsequent resolution of the underlying cause)? This is a classic example of “the best predictor of future behavior is past behavior.”
We, as service providers, frequently hear “think medical first,” but what exactly does this mean?
- One way is to observe if there is an area or region of the body focused on by the acute behavior. For Ron, his behavior of bringing his knees to his chest compresses his abdomen, which can give a clue to an area that should be focused on.
- Additionally, is there a logical reason for the behavior? For Ron, bringing his knees to his chest in a seated position, although “odd,” can relieve pressure by promoting gas relief and/or a bowel movement.
- Another way of thinking from a medical point of view is noting the connection between avoiding food and not having bowel movements. In this scenario, I often think, “Well, something is going on between when it goes in and when it comes out. Should we start following the path from the bottom or the top?!”
For Ron, behavioral interventions to manage future constipation could include simple communication strategies and toileting logs. If Ron does not currently have an effective means of communicating pain or discomfort, it would be beneficial to teach Ron a basic sign or gesture to assist him in communicating if he does not feel well in any scenario. Regarding toileting logs, keeping simple documentation of bowel movements can help identify potential constipation issues early to prevent more severe gastrointestinal concerns, such as fecal impaction.
Outcome
The nurse knew that Ron had experienced bouts with constipation in the past and that he usually had similar behaviors when he did. After confirming a rectal fecal impaction, his physician recommended an enema and a short-term laxative. He also recommended a consultation with a dietician to increase the fiber content of his diet slowly and included the recommendation to concurrently increase fluid intake as his fiber intake increased. This is important as increasing fiber alone could make constipation worse. Within a few weeks, his fiber and fluid intake had increased to the recommended range, and his recurrent bouts of constipation resolved. Not surprisingly, his overall demeanor was more positive as well.
The Authors
Risley “Ley” Linder
Ley is a Board-Certified Behavior Analyst with an academic and professional background in gerontology and applied behavior analysis. Ley’s specialties include behavioral gerontology and the behavioral presentations of neurocognitive disorders, in addition to working with high-management behavioral needs for dually diagnosed persons with intellectual disabilities and mental illness. He is an officer on the Board of Directors for the National Task Group on Intellectual Disabilities and Dementia Practices, works closely with national organizations such as the National Down Syndrome Society, and is the owner/operator of Crescent Behavioral Health Services based in Columbia, SC.
Dr. Craig Escudé
Dr. Craig Escudé is a board-certified Fellow of the American Academy of Family Physicians, the American Academy of Developmental Medicine, and President of IntellectAbility. He has more than 20 years of clinical experience providing medical care for people with IDD and complex medical and mental health conditions. He is the author of “Clinical Pearls in IDD Healthcare” and developer of the Curriculum in IDD Healthcare,” an eLearning course used to train clinicians on the fundamentals of healthcare for people with IDD.