Making Friends Using Person-Centered Practices

By Patrick Lane
One of the best things about being a person is having friends.
Some of us have a lot and others have a few, but we all need friends. Yet so many of the people we support have lives marked with loneliness and isolation. Often anxiety, depression, overreactions, and even health risks are rooted in not having at last one or two good friends.
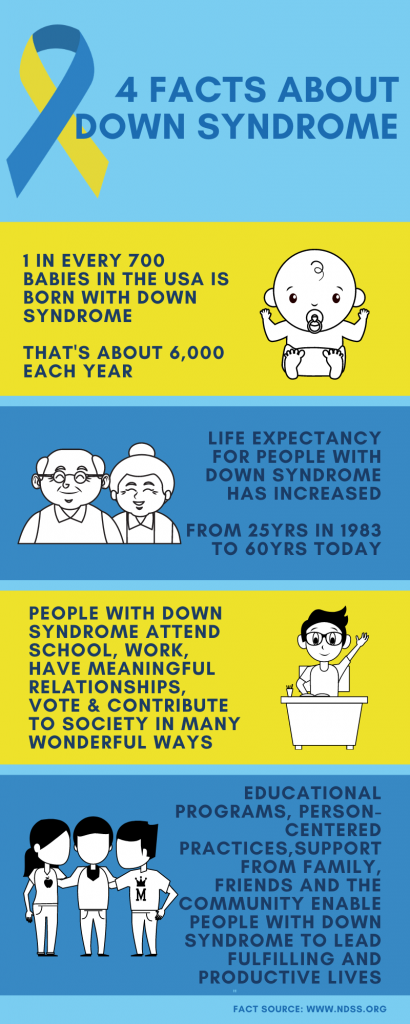
Along with helping people balance Important To with Important For and using common language instead of “disability-speak”, Person Centeredness is about helping people with disabilities with the essential human need of building friendships. The question that follows seems to be: How do we do that?
There is no textbook answer, but here is a good way to get started: simply list the steps you take in your life to make friends. After all, Person-Centeredness is just “human stuff” broken into smaller pieces so others can know where to help and in a way that is appreciated.
Helping people with disabilities works much the same as how you would like to be helped.
For me, I like to meet people with common interests. Once I’m in a setting with those folks, I may strike up a conversation with someone. If that goes well, I’ll ask for their number. Later I’ll text or call and plan a time to get together with my new friend and possibly others. The friendship may grow or fade, and it’s likely that I’ll connect with others and begin making more friends.
If someone were helping me, they would simply break those steps down and add support where needed. This could be done by arranging transportation, making purchases, helping me understand what is being communicated, or respecting the group’s social norms. That being said, I wouldn’t want the person helping me to take over or make my decisions, and I’d only want help where it’s needed. If we differed on how that someone would help me, we’d keep negotiating until we found a way that worked.
The process of making friends will differ from person to person. Navigating this process will go hand-in-hand with properly gauging where help is needed and how much help to offer. This is worked out with some trial, error, and learning.
You should record what you learn in a Learning Log, so when someone else comes along to help later the same mistakes won’t be repeated. You may find that you don’t know what kind of people they prefer to be friends with. To resolve this, people who support should look at current or past relationships. Refer to their Relationship Map to see what personality traits are shared among those who are close to the person.
If we are willing to try, we can help people with disabilities escape loneliness, and isolation and the negative effects that follow. If we are willing to learn, we really can help make someone’s life better because we helped them make real friends. And after all, one of the best things about being a person is having friends.