Identifying Hearing and Vision Changes
Identifying Vision and Hearing Changes in People with IDD as They Age
AS MOST OF THIS AGE, WE BEGIN TO EXPERIENCE CHANGES IN OUR VISION AND HEARING. I 7.5 MIN
Written by Craig Escudé, MD, FAAFP, FAADM
As most of this age, we begin to experience changes in our vision and hearing. We commonly associate aging with difficulty seeing closer and difficulty hearing. Some with intellectual and developmental disabilities may have trouble communicating these changes, and the first signs of them may appear as changes in their behavior. Let’s talk about what we might observe that could indicate a vision or hearing change in someone with an intellectual disability.

Vision
Several conditions can cause visual changes as we age:
- Presbyopia – difficulty seeing close due to a decreased lens elasticity, which affects our ability to focus.
- Age-related macular degeneration
- Glaucoma
- Cataracts
- Diabetic retinopathy
In a person who is unable to communicate changes in their vision using words, we might observe behaviors that involve:
- Frequent touching or rubbing of their eyes
- Finger flapping in front of their eyes
- Gazing at bright lights
- A change in their usual head positions including moving their head but not their eyes to look at things
- Frequent shaking of their head.
- Visual changes might also present as a person moving their head in a circular motion to find an area of better focus.
- The person may also put their hand over one eye if they cannot see out of it clearly.
- Frequent frowning as an attempt to strain to see better.
- Frequent blinking may also be noted.
- Problems such as a cataract may cause someone to avoid bright lights or to blink heavily at bright lights.
You might also see dramatic changes in a person’s behavior. They may become upset or anxious for no apparent reason or startled by noises because their vision is affected, and they can’t see what’s happening around them.
Other indications of visual loss include:
- Not recognizing people unless spoken to because they cannot visually recognize the person.
- Not making eye contact
- Staring for long periods at someone as they are trying to figure out who they are.
- Being startled when approached without being warned.
- Favoring areas of bright lights or moving objects to areas with better lighting.
- Having trouble making out items that are similar in color, such as a white plate on a white tablecloth.
You may also see a change in the person’s activities where they:
- Avoid close-up work because they can no longer see it well
- May draw tiny pictures or very large pictures
- May seem to see bright colors better than dark ones
- Appear to have a short attention span
- Exhibit poor self-care skills because they can no longer see themselves clearly.
- Seem anxious or unwilling to walk alone
- Fall or crash into objects
- Seem clumsy or uncoordinated.These changes may be particularly noted in areas that are poorly lit.
- Mistake dark areas in flooring, such as a dark rug on a light-colored floor, as a hole or a step, and may be afraid to walk in that area.

Hearing
Hearing loss can come from different causes. One more common and easily treatable cause is cerumen impaction, also known as excessive ear wax. This can usually easily be removed by a clinician.
Other problems include:
- Ear infections
- Sensory-neural hearing loss
- Damage to the hair cells that sense sound waves
- A combination of different causes.
Presbycusis is age-related hearing loss due to the loss of the tiny hair cells and the interior of the ear that pick up sound waves.
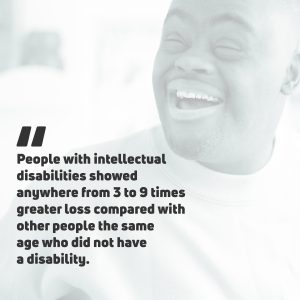
In one study of hearing loss in people with and without disabilities, people with intellectual disabilities showed anywhere from three to nine times greater loss compared with other people the same age who did not have a disability. Recognizing hearing loss earlier rather than later can not only help people remain more engaged in life but can help reduce the risk of dementia. People who experience hearing loss are significantly more likely to experience cognitive decline and dementia than people who do not experience hearing loss. And correcting that hearing loss early can have a significant, positive impact on the outcome.
People who experience hearing loss as they get older may:
- Seem distracted, particularly in noisy areas.
- Turn up the volume on the television or radio louder than usual.
- Not seem to understand conversations and ask people to repeat themselves.
- Become disengaged from others and appear less interested in activities they used to enjoy.
- Be startled when someone “suddenly” appears in from of them because they did not hear them come into the room.
- Not seem to follow requests, such as “Let’s go eat,” because they cannot hear it.
What To Do
Be aware of any changes you see in people around you who may have difficulty communicating using words. An appropriate healthcare professional should evaluate a person who exhibits visual or hearing loss signs to determine if these causes are treatable or if assistive devices, such as glasses or hearing aids, could be helpful. Early treatment can help people remain active and engaged in life, contributing to a better overall quality of life.